Therapist Covered By Insurance

Mental health has been a growing concern worldwide, with an increasing number of individuals seeking professional support to navigate various challenges. In recent years, there has been a significant shift towards prioritizing mental well-being, and one crucial aspect of this movement is ensuring that therapy services are accessible and affordable. This article delves into the topic of therapists covered by insurance, exploring the landscape of mental health coverage, the benefits it offers, and how it impacts individuals seeking therapeutic support.
The Landscape of Mental Health Insurance Coverage

The availability and extent of mental health coverage vary significantly depending on the country, healthcare system, and individual insurance plans. In many developed nations, there has been a push towards integrating mental health services into mainstream healthcare, recognizing the importance of early intervention and ongoing support.
In the United States, for instance, the Mental Health Parity and Addiction Equity Act (MHPAEA) was enacted to ensure that insurance plans offering mental health benefits provide coverage comparable to that of medical and surgical benefits. This means that if a plan includes mental health services, they must be covered at a similar level to physical health services, in terms of cost and access.
Insurance Plans and Mental Health Benefits
Insurance plans can vary greatly in their coverage of mental health services. Some plans may offer comprehensive coverage, including a certain number of therapy sessions per year, while others may have more limited benefits, such as only covering therapy for specific diagnoses or requiring a higher copay.
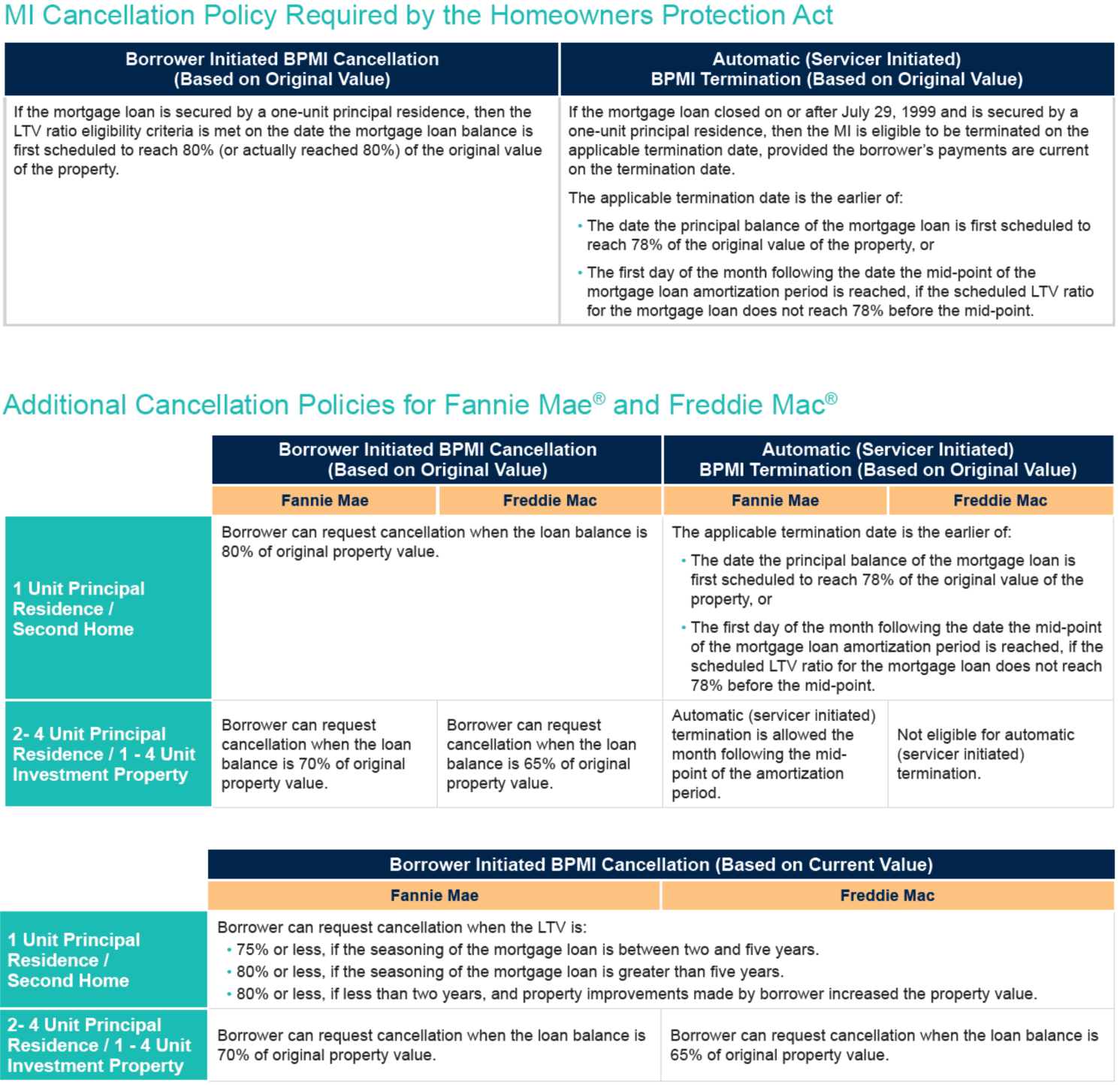
| Insurance Type | Mental Health Coverage |
|---|---|
| Private Health Insurance | Varies widely based on the plan. Some offer extensive coverage, while others may have limited or no mental health benefits. |
| Employer-Provided Insurance | Often includes mental health coverage, but the extent of benefits can vary between employers and their chosen insurance providers. |
| Government-Funded Insurance | May provide more standardized mental health coverage, with certain minimum requirements, but the specifics can differ between regions and programs. |

It's essential for individuals to carefully review their insurance plans to understand the specifics of their mental health coverage, including any limitations, copays, or out-of-pocket maximums.
The Benefits of Insurance Coverage for Therapy

Having therapy covered by insurance can provide numerous advantages for individuals seeking mental health support.
Financial Accessibility
One of the most significant benefits is financial accessibility. Therapy sessions can be costly, with private therapists often charging upwards of $100 per hour. For many, this expense is a barrier to accessing the help they need. With insurance coverage, individuals can access these services at a reduced cost or sometimes even for free, making therapy a more feasible option.
This financial accessibility can be life-changing for those struggling with mental health issues, allowing them to focus on their well-being without the added stress of financial strain.
Reduced Stigma
Insurance coverage for therapy also plays a role in reducing the stigma associated with mental health. When therapy is included as a standard healthcare benefit, it sends a powerful message that mental health is just as important as physical health. This normalization can encourage more people to seek help without feeling judged or marginalized.
Continuity of Care
Insurance coverage often provides a pathway for individuals to receive ongoing care. Many mental health conditions require long-term treatment and support, and insurance coverage ensures that individuals can access this continuity without facing financial barriers.
Additionally, insurance plans may offer a network of therapists, allowing individuals to choose from a range of professionals who are familiar with the insurance process and can provide seamless care.
Challenges and Considerations
While insurance coverage for therapy is a significant step forward, there are still challenges and considerations to keep in mind.
Limitations and Exclusions
Insurance plans often come with limitations and exclusions. For instance, some plans may only cover a certain number of therapy sessions per year or may require pre-authorization for ongoing treatment. Understanding these limitations is crucial to managing expectations and ensuring access to the necessary care.
Finding an In-Network Therapist
When utilizing insurance coverage for therapy, individuals often need to find a therapist who is part of their insurance network. This can be a challenge, especially in areas with limited mental health professionals. It may require some research and flexibility in terms of preferred therapists or locations.
Out-of-Pocket Costs
Even with insurance coverage, there are often out-of-pocket costs associated with therapy. These can include copays, deductibles, and any costs that exceed the plan’s coverage limits. It’s important for individuals to be aware of these potential expenses and plan accordingly.
Future Implications and Advancements
The integration of mental health coverage into insurance plans is an ongoing process, and there is room for improvement and expansion.
Expanding Coverage
Advocacy efforts are pushing for more comprehensive mental health coverage, including increasing the number of covered sessions and reducing or eliminating copays. This would make therapy more accessible and affordable for a wider range of individuals.
Telehealth and Online Therapy
The rise of telehealth services, particularly during the COVID-19 pandemic, has opened up new avenues for mental health support. Online therapy platforms and telehealth services can provide convenient and accessible options for individuals, especially those in rural or remote areas. Insurance coverage for these services is an area of focus, ensuring that individuals can access therapy regardless of their location.
Specialized Treatment Options
As our understanding of mental health evolves, so too should insurance coverage. This includes expanding coverage to include specialized treatment options, such as art therapy, equine-assisted therapy, or other alternative therapeutic approaches that may benefit specific individuals.
Can I choose my own therapist if they are not in-network with my insurance provider?
+
While it is ideal to find an in-network therapist to ensure coverage, you may still have options. Some insurance plans allow for out-of-network reimbursement, where you pay the therapist directly and then submit a claim to your insurance provider for reimbursement. However, the reimbursement process can be complex, and it’s important to check with your insurance provider about their specific policies and requirements.
What happens if I exceed the number of covered therapy sessions in my insurance plan?
+
If you exceed the covered sessions, you may still be able to continue therapy, but it will likely be at an increased out-of-pocket cost. Some insurance plans offer a limited number of additional sessions at a higher copay or require pre-authorization for ongoing treatment. It’s important to discuss these options with your therapist and insurance provider to understand the financial implications.
Are there any mental health conditions that are typically excluded from insurance coverage for therapy?
+
Insurance plans can have exclusions for certain mental health conditions, especially if they are considered pre-existing or if the plan has specific limitations. It’s important to review your insurance policy carefully and, if necessary, discuss any concerns with your insurance provider. In some cases, advocacy groups or legal support may be able to assist in challenging unfair exclusions.
How can I find a therapist who accepts my insurance?
+
You can start by checking your insurance provider’s website or calling their customer service line. Many insurance providers maintain directories of in-network therapists. Additionally, you can search for therapists online and filter by insurance acceptance. Some therapy platforms also allow you to search for therapists based on insurance coverage.