Medical Carrier Contracts

The Complex Landscape of Medical Carrier Contracts: Navigating the Industry’s Legal Framework

In the intricate world of healthcare, medical carrier contracts play a pivotal role, shaping the relationships between healthcare providers, insurance companies, and patients. These contracts are the backbone of the industry, governing the flow of services, payments, and patient care. Understanding their intricacies is essential for healthcare professionals, administrators, and legal experts alike. This article delves deep into the legal and practical aspects of medical carrier contracts, offering a comprehensive guide to navigate this complex landscape.
Understanding the Fundamentals: What are Medical Carrier Contracts?

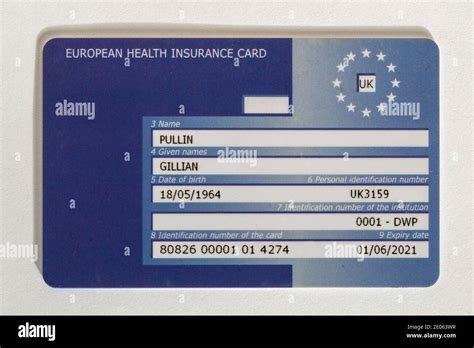
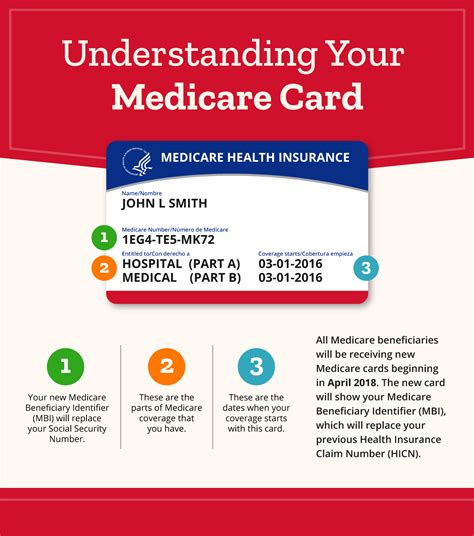
Medical carrier contracts, also known as provider agreements or payer contracts, are legally binding agreements between healthcare providers (doctors, hospitals, clinics) and insurance companies (payers). These contracts outline the terms and conditions under which healthcare services will be delivered and reimbursed. They are the bridge that connects the healthcare delivery system with the financial system, ensuring that patients receive the necessary care while providers are compensated fairly.
Key Components of Medical Carrier Contracts
Network Participation and Provider Status: Contracts specify whether the provider is in-network or out-of-network for the insurance plan. In-network providers agree to accept the payer’s negotiated rates and follow certain guidelines, while out-of-network providers may have more flexibility but often face higher reimbursement hurdles.
Reimbursement Rates and Methods: This section details how and when providers will be paid. It covers fee schedules, allowance rates, and payment methodologies. Reimbursement can be based on various models, including fee-for-service, capitation, or a combination of both.
Utilization Management and Quality Assurance: Contracts often include provisions for utilization review, prior authorization, and quality improvement initiatives. These measures help ensure that services provided are medically necessary, cost-effective, and of high quality.
Credentialing and Licensing: Providers must meet certain standards to be included in the payer’s network. Contracts outline the credentialing process, including requirements for licenses, certifications, and ongoing training.
Term and Termination: Medical carrier contracts typically have a defined term, after which they can be renewed or terminated. Termination clauses specify the grounds for contract termination and the notice period required.
The Legal and Regulatory Environment
Medical carrier contracts are governed by a complex web of laws and regulations, including federal and state statutes, agency regulations, and common law. The Affordable Care Act (ACA), for instance, has significantly influenced the healthcare industry, impacting contract terms and the overall landscape of healthcare delivery and payment.
Key Legal Considerations
Antitrust Laws: Healthcare providers must be mindful of antitrust laws, which prohibit collusion and price-fixing. When negotiating contracts, providers must ensure they do not engage in activities that could be seen as anti-competitive.
Patient Privacy and Data Security: With the increasing digitization of healthcare, contracts must address patient privacy and data security. The Health Insurance Portability and Accountability Act (HIPAA) sets the standard for protecting patient information, and contracts should align with these regulations.
Fraud and Abuse: Healthcare fraud is a serious concern, and contracts must include provisions to prevent and detect fraudulent activities. This includes measures to ensure accurate billing and coding, as well as mechanisms for reporting and addressing suspected fraud.
Negotiating Medical Carrier Contracts
Negotiating medical carrier contracts is a delicate balance between securing favorable terms for providers while also maintaining a collaborative relationship with payers. The negotiation process can be complex and time-consuming, often requiring the expertise of legal and financial advisors.
Key Strategies for Effective Negotiation
Data-Driven Approach: Negotiations should be backed by comprehensive data analysis. This includes understanding the payer’s market share, the provider’s patient population, and the competitive landscape.
Collaborative Relationship: Building a collaborative relationship with payers can lead to more successful negotiations. This involves understanding the payer’s goals and challenges and working together to find mutually beneficial solutions.
Clear Communication: Effective communication is key. Providers should clearly articulate their expectations, needs, and the value they bring to the payer’s network.
Flexibility and Adaptability: Being flexible and adaptable is crucial. Providers should be prepared to negotiate on various aspects of the contract, while also knowing their deal-breakers and non-negotiables.
Performance Analysis and Contract Management

Once a medical carrier contract is in place, ongoing performance analysis and contract management are essential to ensure the contract remains beneficial for all parties involved. This involves regular reviews, data analysis, and proactive management.
Performance Analysis Techniques
Claims Analysis: Regularly reviewing claims data can help identify trends, potential issues, and areas for improvement. This includes analyzing denial rates, payment timelines, and the accuracy of reimbursements.
Network Utilization: Tracking network utilization can provide insights into patient flow and provider performance. It helps identify gaps in service delivery and areas where providers may need additional support or resources.
Quality Assurance: Continuous quality assurance measures ensure that the services provided meet the necessary standards. This includes regular audits, performance reviews, and patient satisfaction surveys.
| Performance Metric | Measurement |
|---|---|
| Denial Rate | Percentage of claims denied by the payer |
| Payment Timeliness | Average days to receive payment from the payer |
| Quality of Care | Patient satisfaction scores, clinical outcome measures |

Future Implications and Industry Trends
The landscape of medical carrier contracts is constantly evolving, influenced by technological advancements, changing regulations, and shifting market dynamics. Understanding these trends is crucial for providers and payers to stay ahead of the curve and adapt their strategies accordingly.
Industry Insights and Predictions
Value-Based Care: There is a growing shift towards value-based care models, where providers are reimbursed based on patient outcomes rather than the volume of services delivered. This trend is expected to continue, driving a need for more sophisticated performance measurement and quality assurance systems.
Telehealth and Digital Health: The COVID-19 pandemic has accelerated the adoption of telehealth and digital health solutions. Medical carrier contracts will need to adapt to incorporate provisions for these new delivery models, including reimbursement rates and data privacy considerations.
Data Analytics and AI: Advanced data analytics and artificial intelligence are transforming the healthcare industry. These technologies can be leveraged to optimize contract negotiations, improve performance analysis, and enhance overall contract management.
Consumer-Driven Healthcare: As consumers become more involved in their healthcare decisions, there is a growing trend towards consumer-driven healthcare models. Medical carrier contracts may need to evolve to accommodate consumer-directed benefits and flexible spending accounts.
Frequently Asked Questions
How often should medical carrier contracts be reviewed and updated?
+Medical carrier contracts should be reviewed and updated at least annually to ensure they remain current and aligned with the latest industry trends and regulations. However, more frequent reviews may be necessary if there are significant changes in the healthcare landscape, such as new laws or major technological advancements.
What are some common challenges faced during the negotiation process?
+Common challenges include differing expectations between providers and payers, complex regulatory environments, and the need for detailed data analysis to support negotiation positions. Additionally, the time and resource-intensive nature of the negotiation process can be a significant challenge.
How can providers ensure they are getting fair reimbursement rates?
+Providers should conduct thorough market research to understand the competitive landscape and benchmark their rates against industry standards. They should also negotiate with multiple payers to leverage their market position and secure favorable terms.