What Is Managed Care Insurance
In the ever-evolving landscape of healthcare, the concept of managed care insurance has emerged as a pivotal element, reshaping the way medical services are delivered and accessed. This innovative model, designed to streamline healthcare delivery and enhance cost efficiency, is a critical aspect of the modern healthcare system. Managed care insurance has become an indispensable tool for both healthcare providers and patients, offering a range of benefits and unique challenges. In this comprehensive exploration, we delve into the intricacies of managed care insurance, uncovering its mechanisms, advantages, and implications for the future of healthcare.
Understanding the Basics of Managed Care Insurance

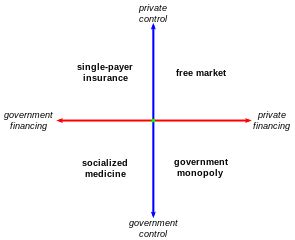
At its core, managed care insurance is a healthcare delivery system that aims to control costs and ensure the quality of patient care by managing various aspects of medical services. This system is designed to provide comprehensive healthcare coverage while controlling costs, ensuring quality, and improving patient outcomes. It is a departure from the traditional fee-for-service model, where patients and healthcare providers had more freedom in choosing treatments and specialists.
The origins of managed care insurance can be traced back to the 1970s when the healthcare industry was grappling with rising costs and an increasing demand for efficient, accessible healthcare services. This period saw the development of innovative models to address these challenges, with managed care emerging as a leading solution. Managed care insurance gained prominence as a cost-effective and quality-driven alternative to the traditional healthcare system.
The fundamental principle of managed care insurance is to establish a network of healthcare providers, including hospitals, clinics, and specialists, who agree to provide services at negotiated rates. This network is then made available to members of the insurance plan, who benefit from reduced costs and a coordinated care approach. The system emphasizes prevention, early intervention, and the efficient use of healthcare resources to ensure the best possible patient outcomes.
Key Components of Managed Care Insurance
- Pre-authorization and Utilization Review: Managed care plans often require pre-authorization for certain procedures and treatments. This process ensures that the services are medically necessary and appropriate, helping to control costs and prevent unnecessary procedures.
- Provider Networks: The network of healthcare providers is a critical aspect of managed care. Members have access to a designated group of providers who have agreed to offer services at negotiated rates, providing cost savings and a coordinated approach to care.
- Co-pays and Deductibles: Managed care plans typically involve out-of-pocket costs for members, such as co-pays for office visits or deductibles for certain procedures. These costs are often lower than in traditional fee-for-service plans, making healthcare more affordable for members.
- Wellness and Preventive Care: Managed care places a strong emphasis on preventive care and wellness programs. By encouraging regular check-ups, screenings, and health education, the system aims to catch potential health issues early, reducing the need for more expensive treatments later.
- Case Management: This aspect of managed care involves the coordination of complex or long-term healthcare needs. Case managers work with patients and their families to ensure that the necessary services are provided in a timely and efficient manner, improving overall patient outcomes.
| Managed Care Type | Description |
|---|---|
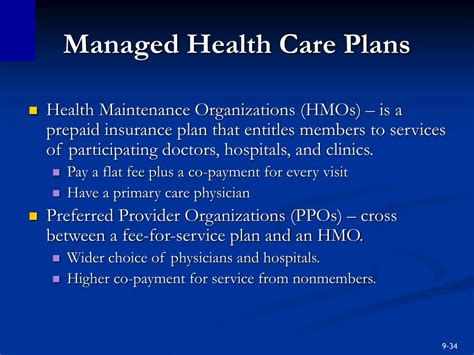
| Health Maintenance Organizations (HMOs) | HMOs require members to choose a primary care physician (PCP) within the network. The PCP acts as a gatekeeper, referring members to specialists within the network. HMOs often have the lowest out-of-pocket costs but may limit member choice. |
| Preferred Provider Organizations (PPOs) | PPOs offer members more flexibility in choosing healthcare providers, both within and outside the network. While members may pay more for out-of-network services, they have the freedom to choose their providers without referrals. |
| Point-of-Service (POS) Plans | POS plans combine features of HMOs and PPOs. Members typically choose a PCP and receive in-network benefits, but they can also access out-of-network services with higher out-of-pocket costs. |
The Benefits and Challenges of Managed Care Insurance

Managed care insurance has revolutionized the healthcare landscape by offering a range of benefits to both patients and healthcare providers. However, like any system, it also presents unique challenges that must be carefully navigated.
Advantages of Managed Care Insurance
- Cost Control: One of the primary advantages of managed care insurance is its ability to control healthcare costs. By negotiating rates with healthcare providers and encouraging the use of cost-effective treatments, managed care plans can offer more affordable premiums to members.
- Improved Access to Care: Managed care insurance has made healthcare more accessible to a broader population. With a network of providers and coordinated care, members can easily locate and access the healthcare services they need, reducing barriers to care.
- Quality Assurance: The focus on quality is a key strength of managed care. By implementing utilization review processes and emphasizing preventive care, managed care plans ensure that members receive appropriate and timely treatments, improving overall healthcare outcomes.
- Efficient Utilization of Resources: Managed care encourages the efficient use of healthcare resources. By coordinating care and reducing unnecessary procedures, the system helps prevent waste and ensures that resources are directed towards the most effective treatments.
- Wellness and Preventive Care: Managed care plans often place a strong emphasis on wellness and preventive care. This proactive approach to healthcare can lead to better health outcomes, reduced disease burden, and lower long-term healthcare costs.
Challenges and Considerations
- Limited Provider Choice: One of the common criticisms of managed care is the potential limitation on provider choice. Members may be required to choose from a network of providers, which can be restrictive, especially for those with specialized healthcare needs.
- Pre-authorization and Paperwork: The pre-authorization process, while beneficial for cost control, can be time-consuming and cumbersome. The paperwork involved in managed care plans can be a burden for both providers and patients, adding to administrative complexities.
- Potential for Underutilization: While managed care aims to reduce unnecessary procedures, there is a risk of underutilization of services. Some members may hesitate to seek necessary care due to concerns about costs or the pre-authorization process, potentially leading to delayed or inadequate treatment.
- Provider Reimbursement: The negotiated rates between providers and managed care organizations can sometimes be a point of contention. Providers may feel that the rates are too low, which can impact their willingness to participate in the network and potentially affect the quality of care provided.
- Changing Healthcare Needs: As healthcare advances and new treatments become available, managed care plans must adapt to ensure they can provide access to the latest, most effective treatments. Keeping up with these advancements is a continuous challenge for managed care organizations.
Managed Care Insurance: A Comprehensive Analysis
Managed care insurance has emerged as a critical component of the modern healthcare system, offering a unique approach to healthcare delivery and cost management. This system, with its focus on coordinated care, cost control, and quality assurance, has revolutionized the way healthcare services are accessed and delivered.
The benefits of managed care insurance are significant. It has made healthcare more accessible and affordable, especially for those with limited resources. By negotiating rates and encouraging the use of cost-effective treatments, managed care plans have helped control the rising costs of healthcare, a critical concern for both individuals and policymakers.
Moreover, the emphasis on preventive care and wellness programs has the potential to transform the healthcare landscape. By catching health issues early and promoting healthy lifestyles, managed care can lead to improved health outcomes and a reduced burden of disease. This proactive approach to healthcare has the potential to save lives and reduce the need for more intensive, expensive treatments down the line.
However, as with any system, managed care insurance is not without its challenges. The limitations on provider choice and the potential for underutilization of services are concerns that must be carefully addressed. The pre-authorization process, while necessary for cost control, can add administrative complexities and potentially deter members from seeking necessary care.
Additionally, the continuous evolution of healthcare, with new treatments and technologies emerging rapidly, presents a challenge for managed care organizations. Keeping up with these advancements and ensuring that members have access to the latest, most effective treatments is a critical task that requires ongoing adaptation and innovation.
Despite these challenges, managed care insurance remains a vital component of the healthcare system, offering a unique and effective approach to healthcare delivery. As the system continues to evolve, addressing these challenges and leveraging its strengths, it has the potential to further improve access to quality healthcare and enhance the overall patient experience.
What is the difference between managed care insurance and traditional fee-for-service insurance?
+Managed care insurance differs from traditional fee-for-service insurance in several ways. In a fee-for-service model, patients have more freedom to choose their healthcare providers and treatments, and providers are reimbursed based on the services rendered. Managed care, on the other hand, involves a network of providers who agree to offer services at negotiated rates. This system emphasizes cost control, quality assurance, and preventive care, providing a more coordinated approach to healthcare.
How does managed care insurance benefit patients?
+Managed care insurance offers several benefits to patients. It provides access to a network of healthcare providers at reduced costs, making healthcare more affordable. The focus on preventive care and wellness programs can lead to better health outcomes and reduced disease burden. Additionally, the coordinated care approach ensures that patients receive appropriate and timely treatments, improving overall healthcare experience.
What are the different types of managed care plans?
+There are several types of managed care plans, including Health Maintenance Organizations (HMOs), Preferred Provider Organizations (PPOs), and Point-of-Service (POS) plans. HMOs require members to choose a primary care physician (PCP) and typically offer lower out-of-pocket costs. PPOs offer more flexibility in provider choice, while POS plans combine features of HMOs and PPOs. Each type has its own advantages and considerations.
How does managed care insurance control costs?
+Managed care insurance controls costs through various mechanisms. It negotiates rates with healthcare providers, encouraging the use of cost-effective treatments. The system also implements utilization review processes to ensure that services are medically necessary and appropriate. Additionally, the emphasis on preventive care can reduce the need for more expensive treatments in the long run.
What are the potential challenges of managed care insurance?
+Managed care insurance faces several challenges. The limitation on provider choice and the potential for underutilization of services are common concerns. The pre-authorization process can be cumbersome, adding administrative complexities. Additionally, keeping up with the rapidly evolving healthcare landscape and ensuring access to the latest treatments is a continuous challenge for managed care organizations.